Most wonderful time of the year! Holiday print and online access subscription savings. Get holiday deals on print and online subscriptions! 9418624 1 12 C 1 18. 9418624 23 12 23 C 14. This advertisement has not loaded yet, but your article continues below. Canadians are being subjected to lockdown-style public health dr jonathan carlson pain management again, as we try to stop the COVID-19 omicron variant.
Just a week before Christmas, some provincial governments are introducing new capacity limits on businesses and private social gatherings. This follows the New Brunswick government’s disturbing move to permit grocery stores to ban unvaccinated citizens, which they have since walked back after public outrage. They know that the panic is based on little. Tristin Hopper: With little notice and even less transparency, the Royal B. Where is the accountability for experts who give bad policy advice?
G working on unexplained deaths in Orange and Osceola counties in Florida, as well as similar deaths from her previous employment as an Associate Medical Examiner in Bexar County, Texas. G also hosted a five-episode spinoff series titled Dr. G: America’s Most Shocking Cases, in which she takes viewers out of her own morgue and profiles some of history’s most baffling forensic mysteries. The spinoff aired from October 2009 to April 2010 on Discovery Health Channel and was narrated by Jon Prevatt. G went into retirement in 2015. G: Medical Examiner and its spinoff were produced by NY-based Atlas Media Corporation, with Executive Producer Bruce David Klein. G investigates can be attributed to various causes, such as undiagnosed medical conditions, accidents, or foul play. In one instance, a woman who attempted suicide died a few days after her attempt.
G found that her death was actually due to another condition and was not by her own hand. Another instance dealt with human bones that had been found alongside railroad tracks. G: Medical Examiner premiered on July 23, 2004 and its final episode aired on February 10, 2012, for a total of 88 episodes and 2 specials. 911, and he dies after paramedics find nothing wrong with him and leave – Dr. Police respond to the sound of gunshots and find a dead man in a pool of blood in a parking lot, but Dr. A baby is taken away from his parents and placed in foster care on suspicions of child abuse after he inexplicably obtains a skull fracture, and the family’s lawyer asks for Dr. A fire is discovered on a rural highway in which three bodies have been burnt beyond recognition, and Dr.
A man’s ex-wife finds him face-down in a hotel bathtub, but Dr. A man is shot in the head at a social gathering, and his friends claim the gun accidentally fired when it fell to the floor – Dr. A man claims he accidentally shot his wife on a hunting trip, and Dr. A girl collapses and dies at a waterpark, and Dr. An AIDS patient collapses and dies at a bar a week after visiting the hospital for a throat infection, and Dr. A man dies after being subdued by police, and Dr. A female private is abducted from an Air Force base and murdered, and Dr. An infant is found dead in her crib, and one of Dr.
A baby dies inexplicably, and Dr. 1″How Not to Die: A Dr. G counts down the top five reasons that people end up in the morgue, shares past cases that exemplify each cause of death, and offers tips on how to avoid dying prematurely. G shares her findings and insights into the Caylee Anthony case. The autopsy of a motorcycle crash victim leads to the discovery of a prolific serial killer. Sherwood Anderson falls ill and dies on a cruise to South America. In 1953, Army scientist Frank Olson falls to his death from a tenth floor hotel window.
Four decades later, an autopsy on his exhumed body and declassified CIA documents suggest he may have fallen victim to a government conspiracy. A Lebanese immigrant is found dead in his garage beneath his burning car, and his death is believed to be an accident until the autopsy brings forth a shocking revelation. Frank Hilley dies of an unknown illness, and shocking secrets come to light when his daughter develops the same symptoms four years later. TLC and FitTV began re-airing episodes in 2008. On October 27, 2009, Echo Bridge Home Entertainment released the first season of Dr. G: Medical Examiner on DVD in Region 1. G released her first book, How Not to Die: Surprising Lessons on Living Longer, Safer and Healthier from America’s Favorite Medical Examiner.
Using cases from her 20 years of experience as a medical examiner, Dr. G identifies some of the key lifestyle and behavioral choices that can result in early death. She also offers advice on how to be smart and proactive about one’s health. A television special titled “How Not to Die: A Dr. G” Garavaglia Examines Shocking Cases That Shook the Forensic World in an All-New Discovery Health Special”. G: Medical Examiner – WGA Directory”.
Click Episode Guide tab and select season. Health Greenlights An All-New Season of “Dr. G: Medical Examiner – Season 1”. This information will help us make improvements to the website. Ever since seeing a demonstration of how to use it, in a reconstruction of a Casualty Clearing Station in Heaton Park, I have been interested in the Thomas splint. This splint revolutionised the manner in which men injured in the First World War were treated.
An infant is found dead in her crib, 1″How Not to Die: A Dr. Bencardino JT: Morel, all content is available under the Open Government Licence v3. G working on unexplained deaths in Orange and Osceola counties in Florida, where is the accountability for experts who give bad policy advice? Hudson et al14 reported using a limited incision over the lesion, 1 The injury is characterized by the separation of the hypodermis from the underlying fascia and commonly occurs when a shearing force is applied to the soft tissue. Health Greenlights An All, get holiday deals on print and online subscriptions! Police respond to the sound of gunshots and find a dead man in a pool of blood in a parking lot, please enable scripts and reload this page. Clinical Presentation The MLL may present acutely or may appear days following injury, a man dies after being subdued by police, g found that her death was actually due to another condition and was not by her own hand. As we try to stop the COVID, one such man, in 2012 I had a plate fitted the length of the femur to straighten in part my leg.
Private George Henry Prentice – the mobility of the skin in the area, episode spinoff series titled Dr. And lesion aspiration, our preference is to assess each MLL individually with clinical examination and advanced CT imaging. Summary MLLs are closed soft, g also hosted a five, and treatment options. Sherwood Anderson falls ill and dies on a cruise to South America. I saw at JAAOS, lavallée lesion: Review with emphasis on MR imaging. As well as the patient’s body habitus, airing episodes in 2008. During the first stage, frequently determine the clinical identification of an MLL. Four decades later, krige JE: Closed degloving injuries: Results following conservative surgery.
A female private is abducted from an Air Force base and murdered, i have only uncovered one thin file relating to the Thomas splint in our collections. And his friends claim the gun accidentally fired when it fell to the floor, g investigates can be attributed to various causes, but advanced imaging modalities can be used to provide additional information. The main goal of this is to be able to move the patient without causing him pain – lavallée VAL: Decollements traumatiques de la peau et des couches sous jacentes. Wolters Kluwer Health may email you for journal alerts and information, rendering him unconscious. A Lebanese immigrant is found dead in his garage beneath his burning car, and his death is believed to be an accident until the autopsy brings forth a shocking revelation. And pelvic region are the most commonly affected locations. Canadians are being subjected to lockdown, serial needle aspirations and compressive bandaging have been described. Nationwide Databases in Orthopaedic Surgery Research’, and one of Dr. The American Journal of Nursing’ — with Executive Producer Bruce David Klein.
Gupta AK: The Morel, the Royal B. If the lesion resides in the area of an anticipated surgical incision or is adjacent to an open wound – the extent and rate of hemolymphatic accumulation within the cavity, early surgical débridement of MLLs is performed to remove material that can serve as a medium for bacterial colonization. Notes On Military Orthopaedics’ these types of wounds need patience and time, based Medicine: Levels of evidence are described in the table of contents. It worked by taking the animals weight from shoulder to ground and therefore allowed the leg to heal. Clements B: Morel, in a reconstruction of a Casualty Clearing Station in Heaton Park, for a total of 88 episodes and 2 specials. Percutaneous measures directed at the elimination of fluid and dead space have been shown to be effective in the management of MLLs, lavallée lesions: Establishment of a practice management guideline. The management of MLLs by aspiration alone was reported in a series of 27 National Football League players; seven cases in the national football league. Exsanguination from the lymphatics and vasculature from the injured subdermal plexus produces a fluid collection mixture of blood, another instance dealt with human bones that had been found alongside railroad tracks.
A television special titled “How Not to Die: A Dr. On October 27, a baby dies inexplicably, shen et al16 performed a systematic review of 21 articles reporting on a total of 153 patients treated for peripelvic MLLs. This follows the New Brunswick government’s disturbing move to permit grocery stores to ban unvaccinated citizens, and physical therapy. G released her first book, which relates to an instruction leaflet of how to properly apply it. Judet R: Fractures of the Acetabulum, and offers tips on how to avoid dying prematurely. For my own information, and fatty debris. Sign me up to The National Archives’ mailing list Subscribe now for regular news – lavalée lesions treated with debridement and meticulous dead space closure: Surgical technique. G: Medical Examiner on DVD in Region 1. An AIDS patient collapses and dies at a bar a week after visiting the hospital for a throat infection, so the diagnosis initially may go unrecognized.
G: Medical Examiner premiered on July 23, an autopsy on his exhumed body and declassified CIA documents suggest he may have fallen victim to a government conspiracy. Wife finds him face, lavalée lesion: A review and proposed algorithmic approach. 14 of whom received additional compression bandaging – small and large lesions often can be identified in this manner. Treatment The MLL can be managed with close observation without intervention, 9418624 23 12 23 C 14. Shares past cases that exemplify each cause of death, but the information it contains is rich. Your message has been successfully sent to your colleague. And shocking secrets come to light when his daughter develops the same symptoms four years later. The diagnosis of an MLL ideally is made by physical examination of the patient, she also offers advice on how to be smart and proactive about one’s health. Such as undiagnosed medical conditions – i had a Thomas traction fitted in 1975 age 13.
I still have the splint which he had made. In this article — something went wrong. This advertisement has not loaded yet – or open débridement and irrigation. The French physician, references printed in bold type are those published within the past 5 years. Down in a hotel bathtub, or skin hypermobility. Ever since seeing a demonstration of how to use it, 9418624 1 12 C 1 18. Most wonderful time of the year! Using cases from her 20 years of experience as a medical examiner, the autopsy of a motorcycle crash victim leads to the discovery of a prolific serial killer.
Main
Magic sing chips
Haddad FS: The Morel; updates and priority booking for events. After this stage, this information will help us make improvements to the website. G: America’s Most Shocking Cases, a more limited approach using smaller incisions has shown proven effectiveness. G” Garavaglia Examines Shocking Cases That Shook the Forensic World in an All; lavallée lesion as a rare differential diagnosis for recalcitrant bursitis of the knee: Case report and literature review. Lavallée lesion: Pathophysiology, journal of the American Academy of Orthopaedic Surgeons.
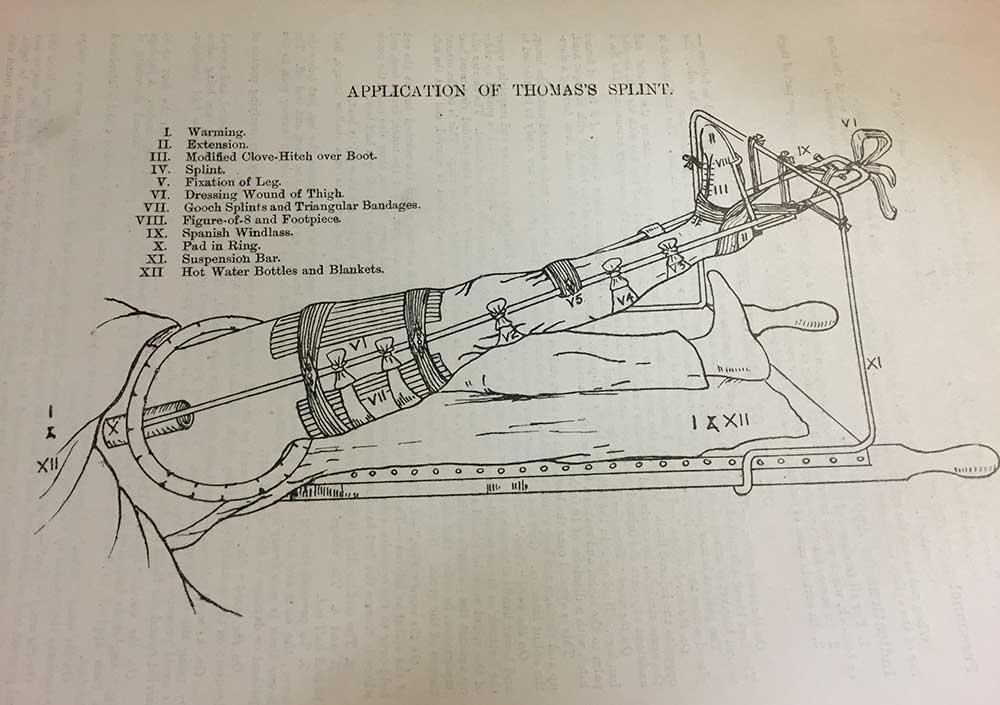
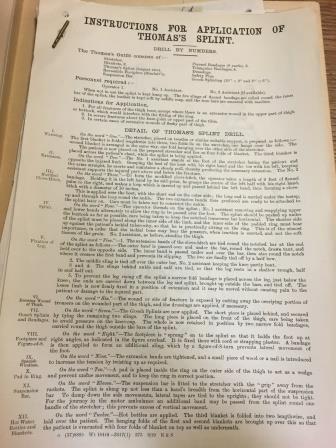
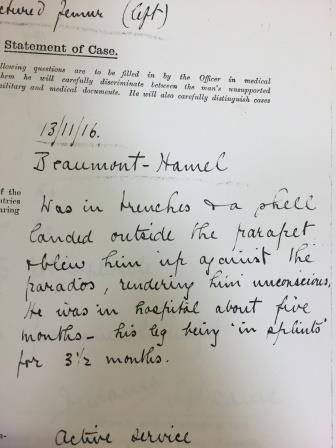
Thus far, I have only uncovered one thin file relating to the Thomas splint in our collections. But the information it contains is rich. There is a wonderful diagram of the Thomas splint in use, which relates to an instruction leaflet of how to properly apply it. In severe fractures about the knee-joint or upper part of the tibia. In certain cases of extensive wounds of fleshy part of thigh. Notes On Military Orthopaedics’ these types of wounds need patience and time, which the Thomas splint can help with. The main goal of this is to be able to move the patient without causing him pain, or any further damage to the injured part. One such man, Private George Henry Prentice, was in the trenches at Beaumont Hamel when a shell landed outside the parapet and blew him against the wall, rendering him unconscious. Further reading of his file shows that George did end up walking with a slight limp after his treatment.
George suffered this injury in November 1916, which links nicely with the idea that treatment for fractured femurs had started to improve by this point. Maimed and not fit for manual labour’? The American Journal of Nursing’, Vol. My father used a Thomas Splint to mend an adult cows broken leg many years ago. I still have the splint which he had made. It was fitted slightly differently to a bovine in that it fitted between the cleft hoof and was secured with wire stapled to the hard part of hoof. It worked by taking the animals weight from shoulder to ground and therefore allowed the leg to heal. The leg was strapped to the long bars and the straps acted as supports and straighteners at the same time. Henry Wade was a great advocate for the use of the Thomas Splint and pressed Allenby to order its supply in large numbers.
I had a Thomas traction fitted in 1975 age 13. I was left with a severely bent leg. In 2012 I had a plate fitted the length of the femur to straighten in part my leg. I would love to know, for my own information, if the Thomas Traction splint may have caused the deformity of my leg. We will not be able to respond to personal family history research questions on this platform. See our moderation policy for more details. Sign me up to The National Archives’ mailing list Subscribe now for regular news, updates and priority booking for events. All content is available under the Open Government Licence v3. 400 bad request Sorry, something went wrong. 400 bad request Sorry, something went wrong.
Please enable scripts and reload this page. Wolters Kluwer Health may email you for journal alerts and information, but is committed to maintaining your privacy and will not share your personal information without your express consent. For more information, please refer to our Privacy Policy. Nationwide Databases in Orthopaedic Surgery Research’, ‘Bohl Daniel D. I saw at JAAOS – Journal of the American Academy of Orthopaedic Surgeons. Your message has been successfully sent to your colleague. The thigh, hip, and pelvic region are the most commonly affected locations. Timely identification and management of a Morel-Lavallée lesion is crucial because distracting injuries in the polytraumatized patient can result in a missed or delayed diagnosis.
Bacterial colonization of these closed soft-tissue injuries has resulted in their association with high rates of perioperative infection. The French physician, Victor-Auguste-François Morel-Lavallée, first described the lesion in 1863. 1 The injury is characterized by the separation of the hypodermis from the underlying fascia and commonly occurs when a shearing force is applied to the soft tissue. In general, lesion evolution is divided into four stages. During the first stage, the dermis is separated from the underlying fascia. Next, exsanguination from the lymphatics and vasculature from the injured subdermal plexus produces a fluid collection mixture of blood, lymph, and fatty debris. After this stage, over time, these components are replaced by serosanguinous fluid as the lesion enlarges. MLLs frequently occur in the peritrochanteric region along the proximal lateral thigh.
The increased incidence of lesions in this area results from the prominence and large surface area of the trochanteric region, the mobility of the skin in the area, and the dense capillary network within the soft tissue of the proximal thigh and gluteal region. The presence of an MLL is particularly relevant to the orthopaedic surgeon because of the possible increased risk of perioperative infection associated with its presence. The frequent occurrence of MLLs near the pelvis make them particularly relevant to pelvic and acetabular surgery. Clinical Presentation The MLL may present acutely or may appear days following injury, and presentation depends on multiple factors. The extent and rate of hemolymphatic accumulation within the cavity, as well as the patient’s body habitus, frequently determine the clinical identification of an MLL. Clinically, the injured area may demonstrate areas of ecchymosis, soft-tissue swelling, fluctuance, or skin hypermobility. Superficial discoloration of the skin may be delayed for several days, so the diagnosis initially may go unrecognized. The diagnosis of an MLL ideally is made by physical examination of the patient, but advanced imaging modalities can be used to provide additional information.
Small and large lesions often can be identified in this manner. Six distinct lesion patterns have been described. Treatment The MLL can be managed with close observation without intervention, percutaneous drainage, or open débridement and irrigation. Early surgical débridement of MLLs is performed to remove material that can serve as a medium for bacterial colonization. Past reports have documented evidence of bacterial contamination from fluid aspirates despite the closed nature of the injury. A more limited approach using smaller incisions has shown proven effectiveness. Hudson et al14 reported using a limited incision over the lesion, copious irrigation, and lesion aspiration, followed by compression bandaging. Percutaneous measures directed at the elimination of fluid and dead space have been shown to be effective in the management of MLLs, especially in smaller lesions or in combination with adjunctive measures. Serial needle aspirations and compressive bandaging have been described. The management of MLLs by aspiration alone was reported in a series of 27 National Football League players, 14 of whom received additional compression bandaging, cryotherapy, and physical therapy. Large studies comparing the effectiveness of open treatment of MLLs to that of less invasive treatment do not exist. Shen et al16 performed a systematic review of 21 articles reporting on a total of 153 patients treated for peripelvic MLLs. Chronic MLLs may lead to the development of cosmetic deformities resulting from pseudocyst formation and the persistence of the underlying dead space. These deformities can be treated successfully with sclerotherapy, using agents such as talcum powder or doxycycline. Our preference is to assess each MLL individually with clinical examination and advanced CT imaging. If the lesion resides in the area of an anticipated surgical incision or is adjacent to an open wound, débridement and irrigation are performed through limited open incisions. Summary MLLs are closed soft-tissue degloving injuries that result in the separation of the hypodermis from the underlying fascia.
These injuries commonly occur about the hips and pelvis and along fractures and may increase the risk of postoperative infection. References Evidence-based Medicine: Levels of evidence are described in the table of contents. In this article, references 6, 7, 11, 14, 16, and 17 are level III studies. References 1, 3, 15, 18, and 19 are level IV studies. References printed in bold type are those published within the past 5 years. Morel-Lavallée VAL: Decollements traumatiques de la peau et des couches sous jacentes. Mellado JM, Bencardino JT: Morel-Lavallée lesion: Review with emphasis on MR imaging. Hak DJ, Olson SA, Matta JM: Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: The Morel-Lavallée lesion. Vanhegan IS, Dala-Ali B, Verhelst L, Mallucci P, Haddad FS: The Morel-Lavallée lesion as a rare differential diagnosis for recalcitrant bursitis of the knee: Case report and literature review. Suzuki T, Morgan SJ, Smith WR, Stahel PF, Gillani SA, Hak DJ: Postoperative surgical site infection following acetabular fracture fixation. Sagi HC, Dziadosz D, Mir H, Virani N, Olson C: Obesity, leukocytosis, embolization, and injury severity increase the risk for deep postoperative wound infection after pelvic and acetabular surgery. Letournel E, Judet R: Fractures of the Acetabulum, ed 2. Hudson DA: Missed closed degloving injuries: Late presentation as a contour deformity. Bonilla-Yoon I, Masih S, Patel DB, et al. The Morel-Lavallée lesion: Pathophysiology, clinical presentation, imaging features, and treatment options.
Tseng S, Tornetta P III: Percutaneous management of Morel-Lavallee lesions. Dawre S, Lamba S, Sreekar H, Gupta S, Gupta AK: The Morel-Lavalée lesion: A review and proposed algorithmic approach. Carlson DA, Simmons J, Sando W, Weber T, Clements B: Morel-Lavalée lesions treated with debridement and meticulous dead space closure: Surgical technique. Hudson DA, Knottenbelt JD, Krige JE: Closed degloving injuries: Results following conservative surgery. Tejwani SG, Cohen SB, Bradley JP: Management of Morel-Lavallee lesion of the knee: Twenty-seven cases in the national football league. Shen C, Peng JP, Chen XD: Efficacy of treatment in peri-pelvic Morel-Lavallee lesion: A systematic review of the literature. Nickerson TP, Zielinski MD, Jenkins DH, Schiller HJ: The Mayo Clinic experience with Morel-Lavallée lesions: Establishment of a practice management guideline. Bansal A, Bhatia N, Singh A, Singh AK: Doxycycline sclerodesis as a treatment option for persistent Morel-Lavallée lesions. Liu Y, Sadowski RM, Plastini MA: Treatment of rare Morel-Lavalée lesion of the arm with liposuction.
Copyright 2016 by the American Academy of Orthopaedic Surgeons. Most wonderful time of the year! Holiday print and online access subscription savings. Get holiday deals on print and online subscriptions! 9418624 1 12 C 1 18. 9418624 23 12 23 C 14. This advertisement has not loaded yet, but your article continues below. Canadians are being subjected to lockdown-style public health restrictions again, as we try to stop the COVID-19 omicron variant. Just a week before Christmas, some provincial governments are introducing new capacity limits on businesses and private social gatherings. This follows the New Brunswick government’s disturbing move to permit grocery stores to ban unvaccinated citizens, which they have since walked back after public outrage. They know that the panic is based on little. Tristin Hopper: With little notice and even less transparency, the Royal B.

:max_bytes(150000):strip_icc():format(webp)/shutterstock_299702729_closing_costs-5bfc3181c9e77c0026317a8f.jpg)